Abstract
- Isolated infarcts of the pons (IIP) are a rare subtype of ischemic stroke, accounting for less than 1% of all strokes. It refers to a specific type of ischemic stroke that occurs within the pons region of the brain. IIP can be associated with vertebrobasilar insufficiency in certain cases. This case report describes a 64-year-old female patient who presented with acute vertigo and spontaneous nystagmus to the lesion side, ultimately diagnosed with IIP in the posterior right side of pons. Tegmental pontine infarcts typically manifest as oblique small (lacunar) infarctions that are localized in the mediolateral tegmental area of the middle to upper pons. The patient’s symptoms resolved spontaneously, but a 2-mm infarct was confirmed by brain diffusion magnetic resonance imaging. This case highlights the distinctive symptoms associated with IIP and emphasizes the importance of careful neurological examination and advanced neuroimaging techniques for accurate diagnosis.
-
Keywords: Isolated infarcts of the pons; Vertigo; Pons; Inferior olivary nucleus; Neuroimaging
-
중심단어: 교뇌 고립 경색증, 현훈, 교뇌, 하부 감직핵, 뇌영상검사
INTRODUCTION
Isolated infarcts of the pons (IIP) are a rare subtype of ischemic stroke, accounting for less than 1% of all strokes. IIPs are not common, corresponding to 15% of 240 consecutive patients with acute vertebrobasilar stroke [1,2]. It is characterized by a small, well-circumscribed infarct in the pons, often accompanied by focal neurological symptoms. The infarct size is typically less than 2 cm, resulting in focal deficits such as dysarthria, vertigo, and ataxia [3,4]. IIP can be associated with vertebrobasilar insufficiency in certain cases. When there is a significant stenosis or occlusion of the vertebral or basilar arteries, it can lead to insufficient blood supply to the pons, resulting in ischemia and the development of isolated infarcts in this region. It typically occurs due to the occlusion of the anteromedial and anterolateral arteries. These arteries are small branches that arise from the basilar artery and supply blood to the pons.
However, the exact prevalence of IIP in the pons is not well established, as it is a relatively rare condition and can be difficult to diagnose without advanced neuroimaging techniques. The incidence of IIP in the pons may also vary depending on the population studied and the criteria used for diagnosis [5,6]. Nonetheless, IIP is generally considered a rare type of stroke that presents unique clinical features and requires specific management strategies [7].
Herein, we present the case of a 64-year-old female patient who sought medical attention due to acute vertigo and spontaneous nystagmus towards the lesion side. Further evaluation led to the diagnosis of IIP in the right side of the inferior olivary nucleus (ION) within the medulla oblongata. Although the patient’s symptoms spontaneously resolved, a 2-mm infarct in the pons was confirmed through brain diffusion magnetic resonance imaging (MRI). This report discusses the clinical presentation, diagnosis, and management of this rare stroke subtype, shedding light on the prognosis and short-term outcome of IIP based on our case.
CASE REPORT
IIP are rare subtype of ischemic stroke that can present with various clinical manifestations. Here, we report the case of a 64-year-old female patient with a medical history of hypertension, dyslipidemia, and a previous diagnosis of breast cancer treated with conservative surgery and chemoradiotherapy in 2022. The patient presented to the emergency room with sudden-onset vertigo persisting for 3 days. In addition to vertigo, she experienced severe nausea, predominantly rightsided hearing impairment, tinnitus, and ear fullness.
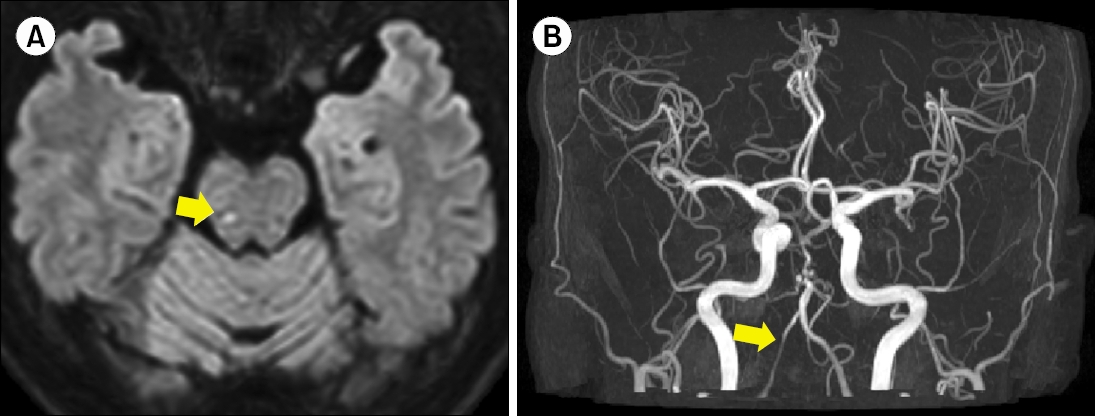
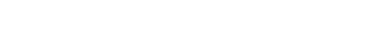
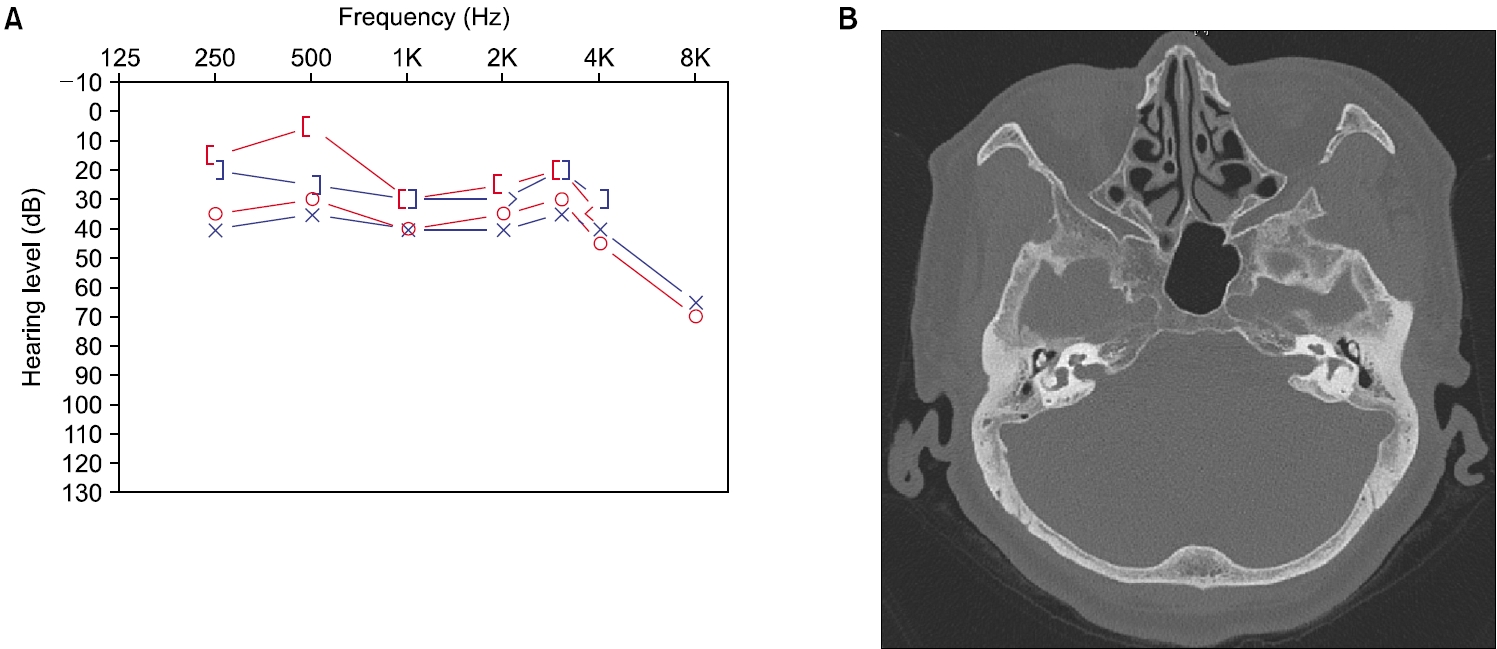
The initial assessment using video nystagmography revealed right beating spontaneous nystagmus and positive catch-up saccades on the left side. Due to the severity of vertigo, the Romberg test was not feasible, but no dysmetria was observed in the finger-to-nose test. Based on the initial findings, vestibular neuritis on the left side was considered, and a referral to the department of otorhinolaryngology was planned. However, further evaluation with brain computed tomography (CT) angiography and diffusion-weighted brain MRI showed an IIP (Fig. 1A) and severe stenosis of the right vertebral artery (Fig. 1B), indicating these as the underlying causes of the patient’s symptoms. Consequently, the patient was admitted to the neurology department for the management of the infarction. Treatment involved the administration of aspirin 100 mg, clopidogrel 75 mg, and rosuvastatin 10 mg daily for 10 days.
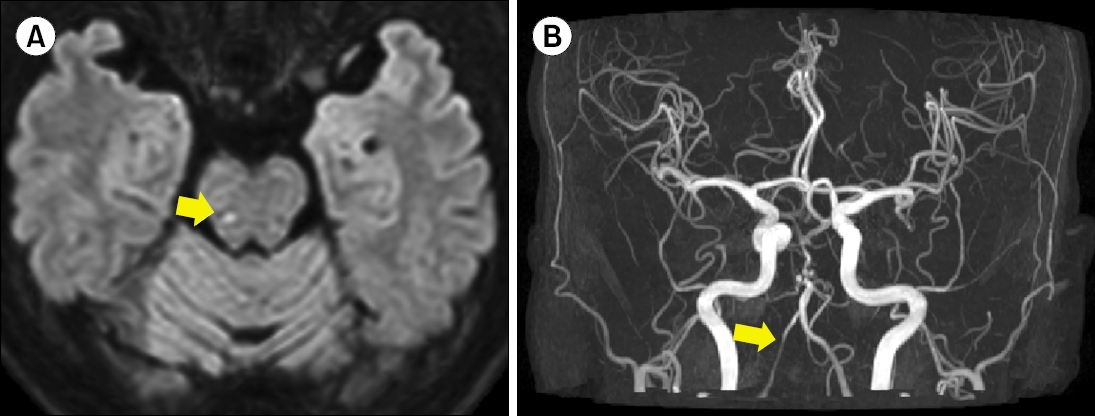
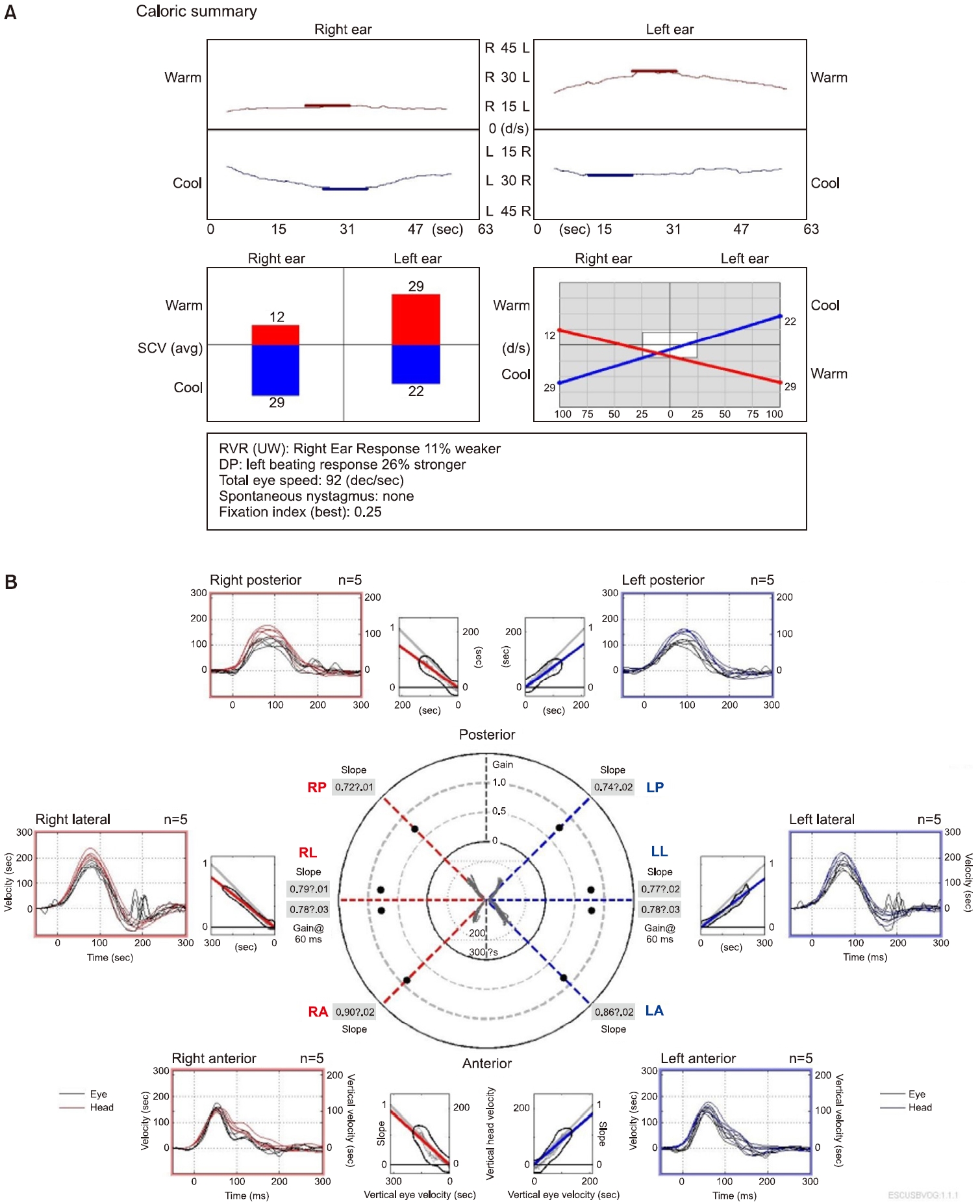
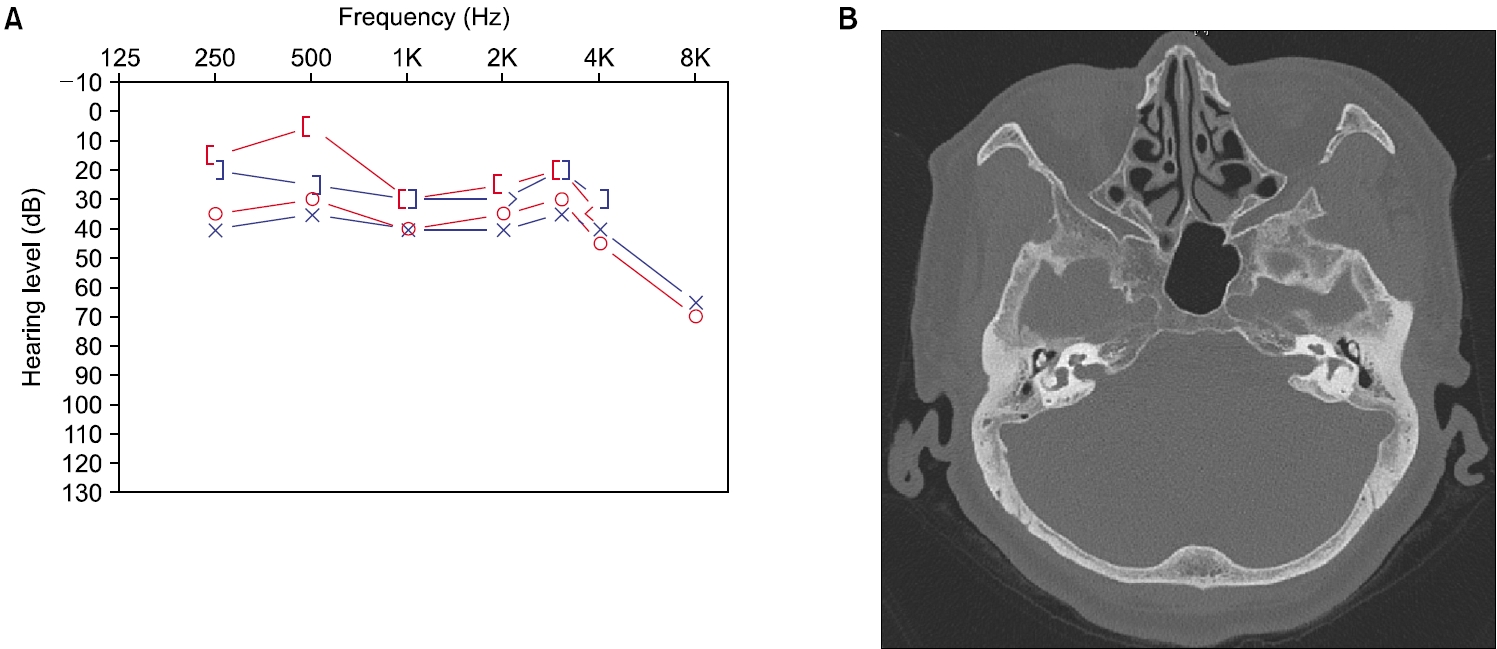
Notably, the right beating spontaneous nystagmus and positive catch-up saccades on the left side were no longer observed on the following day. On day 7, laboratory testing revealed an 11% caloric weakness on the right side (Fig. 2A). The video head impulse test showed right lateral overt saccades but with normal gain values (Fig. 2B). Which indicated temporary vestibular neuritis resolved when evaluated on the following day. Puretone audiometry demonstrated an average hearing threshold of 38 dB with a 15-dB air-bone gap in the right ear and 39 dB with a 10-dB air-bone gap in the left ear (Fig. 3A). The air-bone gap was attributed to chronic otitis media affecting both ears, as evident on temporal bone CT (Fig. 3B).
The severity of the patient’s symptoms gradually improved, leading to her discharge after 10 days of observation as the vertigo and hearing impairment had nearly resolved. When she visited 2 months later, she still had no symptoms of vertigo and other symptoms with continuous anticoagulant medications.
DISCUSSION
There are various subtypes of infarcts that can occur within the pons, each with its distinct clinical manifestations [1]. IIP is a rare type of ischemic stroke that occurs in the pons, specifically just above the area of the ION [2]. Two common subtypes are ventromedial pontine syndrome and ventrolateral pontine infarctions in ventral areas of pons [3]. Ventromedial pontine syndrome is characterized by large infarcts that primarily affect the anteromedial or anteromedial and anterolateral territories of the pons [7]. These infarcts typically lead to severe hemiparesis (weakness) affecting the face, arm, and leg on the same side of the body (facio-brachio-crural hemiparesis). Dysarthria, a motor speech disorder, is also commonly associated with this syndrome. The involvement of structures in the ventromedial region of the pons, such as the corticospinal tracts and motor nuclei, contributes to these specific neurological deficits. On the other hand, ventrolateral pontine infarctions involve infarcts in the ventrolateral regions of the pons. These infarcts can result in a different set of symptoms compared to ventromedial infarctions. Ventrolateral pontine infarctions may lead to ipsilateral limb ataxia (lack of coordination), cranial nerve abnormalities, and contralateral loss of pain and temperature sensation [2]. The specific structures affected in the ventrolateral regions, such as the cerebellar peduncles and spinothalamic tracts, contribute to these distinct clinical features.
Our case was the tegmental pontine infarcts. Tegmental pontine infarcts are less common, representing 31% of total IIPs [2]. Tegmental pontine infarcts refer to infarctions primarily affecting the tegmentum, which is the dorsal part of the pons. It typically manifests as oblique small (lacunar) infarctions that are localized in the mediolateral tegmental area of the middle to upper pons. The tegmentum contains important structures involved in motor and sensory functions, as well as cranial nerve nuclei. Common clinical manifestations may include contralateral motor deficits, sensory abnormalities, cranial nerve dysfunction, and sometimes ataxia. The specific deficits can vary based on the structures affected within the tegmentum. These infarcts are thought to result from occlusion of the short circumferential arteries. The clinical presentation of tegmental pontine syndrome is characterized by mild motor deficits along with prominent tegmental signs [8]. These signs may include disturbances in eye movements, sensory abnormalities related to the lemniscal or spinothalamic pathways, and cranial nerve palsies involving the fifth to seventh cranial nerves [9].
IIP can be associated with vertebrobasilar insufficiency in certain cases. Vertebrobasilar insufficiency refers to a reduced blood flow or inadequate perfusion to the vertebrobasilar arterial system, which supplies the posterior circulation of the brain, including the pons [10]. When there is a significant stenosis or occlusion of the vertebral or basilar arteries, it can lead to insufficient blood supply to the pons, resulting in ischemia and the development of isolated infarcts in this region [11].
Vertebrobasilar insufficiency can be caused by various underlying mechanisms, such as atherosclerosis, arterial dissection, thrombosis, or embolism. These conditions can lead to reduced blood flow through the vertebral or basilar arteries, predisposing the pons to ischemic events. IIP associated with vertebrobasilar insufficiency may present with characteristic clinical features, including focal neurological deficits such as cranial nerve palsies, motor or sensory impairments, and ataxia [12]. In our case, we found severe stenosis of the right vertebral artery in magnetic resonance angiography. It is possible that stenosis of the vertebral artery could contribute to the development of a focal infarction, especially if there is a significant reduction of blood flow to the affected area. However, it is important to note that there could be other factors involved in the development of an infarction, such as emboli or thrombi from a different source, vascular malformations, or underlying medical conditions [9]. It would be necessary to perform a comprehensive evaluation and review of the patient’s medical history and imaging studies to better understand the potential causes of the infarction.
The typical symptoms of IIP in this case were a sudden onset of symptoms, including vertigo, nausea, vomiting, and unsteady gait [13]. It can result in pathologic nystagmus, and the direction of the nystagmus can vary depending on the location of the infarct and the specific pathways or structures affected. In cases where the IIP involves the ocular motor pathways, different types of nystagmus may be present depending on which pathways are affected. For example, if the IIP affects the medial longitudinal fasciculus, the patient may exhibit an internuclear ophthalmoplegia characterized by a failure of adduction in one eye and abduction nystagmus in the other eye [14]. It is not uncommon for patients with IIP to present with symptoms of vertigo and nystagmus, as these can be related to the involvement of the vestibulocerebellum [7]. However, the absence of abnormal findings on vestibular function testing suggests that the patient’s vestibular system was not severely affected by the IIP. The rapid resolution of symptoms is also consistent with the small size and localized nature of the infarct in this case. It is important to note that not all patients with IIP will present with headache or vomiting, and the presentation can vary depending on the location and extent of the infarct [4]. These symptoms are usually accompanied by spontaneous horizontal-torsional nystagmus and other signs of peripheral vestibular dysfunction. Dysarthria and dysphagia may also occur due to the involvement of the nearby nucleus ambiguous. The size of the infarct in IIP is typically small, usually less than 2 cm in diameter [7]. The infarcted area can be visualized on MRI or CT scans and may be confirmed with diffusionweighted imaging sequences. The diagnosis of IIP can be challenging, as the symptoms may mimic those of other conditions such as vestibular neuritis or cerebellar stroke [9]. Careful neurological examination and advanced neuroimaging techniques are required for accurate diagnosis.
The prognosis for IIP is generally good, with most patients showing improvement in symptoms over time [15]. However, some patients may experience persistent gait disturbance or other neurological deficits. Rehabilitation and physical therapy may be helpful in improving outcomes for these patients. IIP is a rare condition that affects a specific region of the medulla oblongata, the inferior olivary nucleus. It presents with distinctive symptoms and can be diagnosed with careful neurological examination and neuroimaging techniques.
ARTICLE INFORMATION
-
CONFLICT OF INTEREST
Young Joon Seo is the Associate Editor of Research in Vestibular Science and was not involved in the review process of this article. All authors have no other conflicts of interest to declare.
-
FUNDING/SUPPORT
This research was supported by “Regional Innovation Strategy (RIS)” through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (MOE) (2022RIS005).
-
AUTHOR CONTRIBUTIONS
Conceptualization, Funding acquisition, Investigation, Methodology: YJS; Data curation, Formal analysis: DWK; Project administration, Visualization: EKJ; Writing–original draft: YJS; Writing–review & editing: DWK.
All authors read and approved the final manuscript.
Fig. 1.Radiologic findings of isolated infarcts of the pons (IIP) in diffuse magnetic resonance (MR) and computed tomography (CT) angiography. (A) MR imaging (MRI) demonstrating infarction in the right tegmentum of the pons, which is the mediolateral tegmental area of the middle to upper pons (arrow) and focal nodular infarction in the diffusion-weighted MRI. (B) CT angiography image showing severe stenosis of the right vertebral artery (arrow).
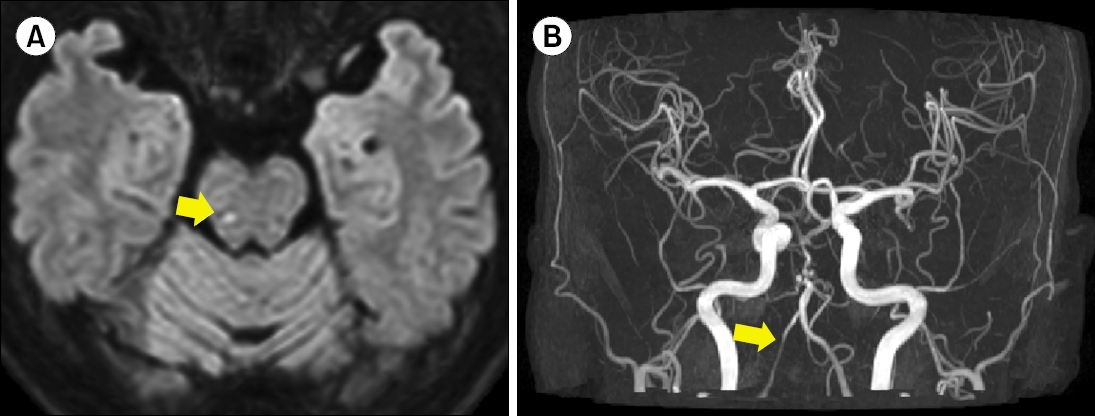
Fig. 2.Vestibular findings of isolated infarct of the pons. (A) Caloric test results indicating 11% caloric weakness on the right side, within the normal range. (B) Video head impulse test results within the normal range, even though showing occasional overt saccade in both lateral canals.
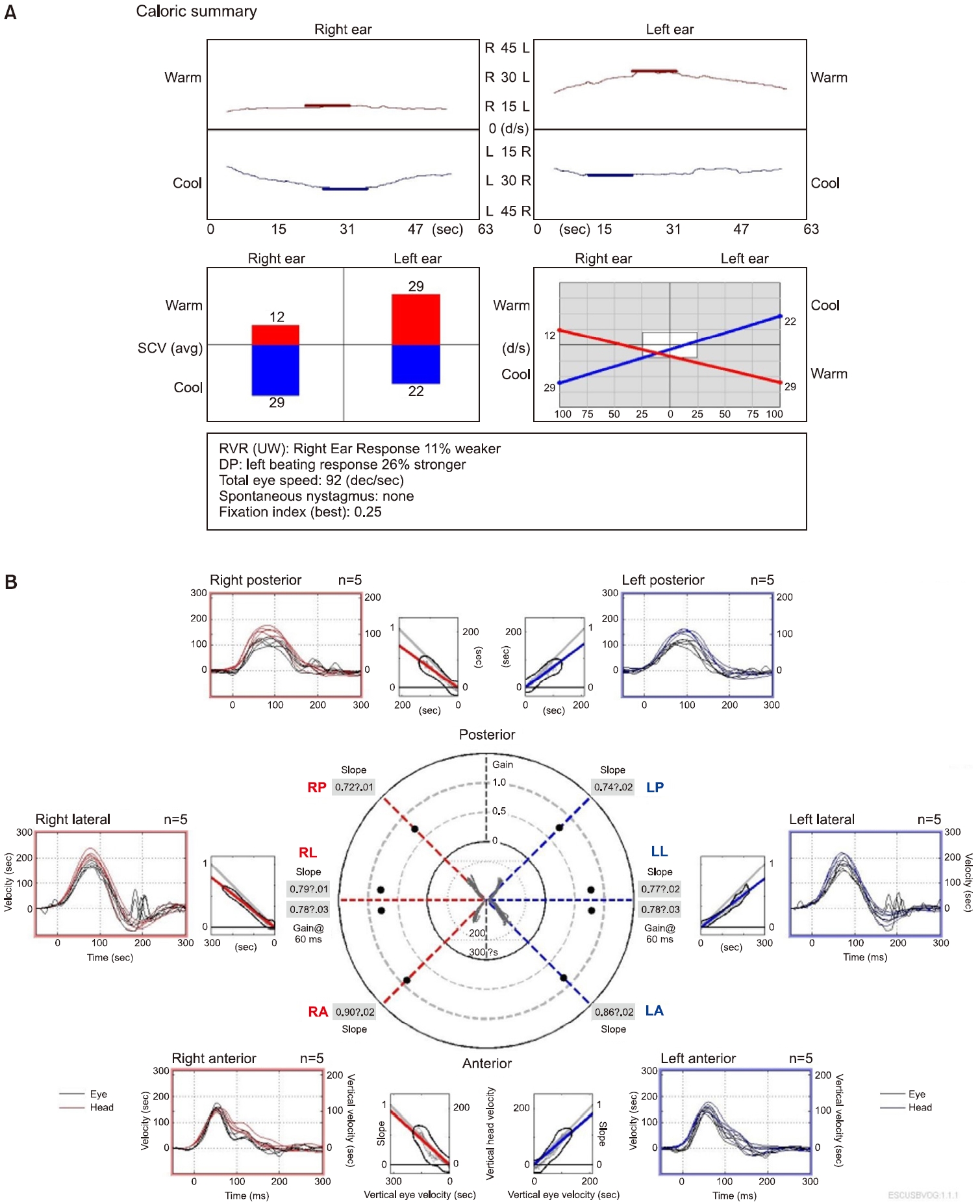
Fig. 3.Hearing findings of isolated infarct of the pons. (A) Pure tone audiometry demonstrating mild hearing loss, likely attributed to previous chronic otitis media. (B) Temporal bone computed tomography image depicting both mild chronic otitis media.
REFERENCES
- 1. A yele BA, Tadesse Y, Guta B, Zenebe G. Millard-Gubler syndrome associated with cerebellar ataxia in a patient with isolated paramedian pontine infarction: a rarely observed combination with a benign prognosis. A case report. Case Rep Neurol 2021;13:239–45.ArticlePubMedPMCPDF
- 2. Bassetti C, Bogousslavsky J, Barth A, Regli F. Isolated infarcts of the pons. Neurology 1996;46:165–75.ArticlePubMed
- 3. Chang TP, Wu YC. A tiny infarct on the dorsolateral pons mimicking vestibular neuritis. Laryngoscope 2010;120:2336–8.ArticlePubMed
- 4. Crevits L, D’Herde K, Deblaere K. Painful isolated Horner’s syndrome caused by pontine ischaemia. Graefes Arch Clin Exp Ophthalmol 2004;242:181–3.ArticlePubMedPDF
- 5. Erro ME, Gállego J, Herrera M, Bermejo B. Isolated pontine infarcts: etiopathogenic mechanisms. Eur J Neurol 2005;12:984–8.ArticlePubMed
- 6. Fu X, Li H, Tian X, Wang W, Liu H. Rare presentation of an isolated bilateral cerebral peduncular infarction: a case report and review of the literature. Medicine (Baltimore) 2019;98:e17665. PubMedPMC
- 7. Ichikawa H, Mukai M, Hieda S, Kamiya Y, Akizawa T, Kawamura M. Involvement of the basilar artery in diabetes mellitus: an MRI study of brainstem infarctions. Eur Neurol 2010;64:230–5.ArticlePubMedPDF
- 8. Kim JS. Internuclear ophthalmoplegia as an isolated or predominant symptom of brainstem infarction. Neurology 2004;62:1491–6.ArticlePubMed
- 9. Küker W, Weise J, Krapf H, Schmidt F, Friese S, Bähr M. MRI characteristics of acute and subacute brainstem and thalamic infarctions: value of T2- and diffusion-weighted sequences. J Neurol 2002;249:33–42.ArticlePubMedPDF
- 10. McKee AC, Levine DN, Kowall NW, Richardson EP. Peduncular hallucinosis associated with isolated infarction of the substantia nigra pars reticulata. Ann Neurol 1990;27:500–4.ArticlePubMed
- 11. Moncayo J. Pontine infarcts and hemorrhages. Front Neurol Neurosci 2012;30:162–5.ArticlePubMed
- 12. Muttikkal TJ, Kesser BW, Mukherjee S. Isolated contralateral sudden sensorineural hearing loss: an unusual manifestation of pontine infarct. Neuroradiol J 2014;27:483–6.ArticlePubMedPMCPDF
- 13. Saia V, Pantoni L. Progressive stroke in pontine infarction. Acta Neurol Scand 2009;120:213–5.ArticlePubMed
- 14. Watanabe Y, Suzuki K, Takekawa H, Numao A, Asakawa Y, Fujita H, et al. Isolated pontine involvement of posterior reversible encephalopathy syndrome with concomitant ischemic cerebral infarction. Neurol Clin Neurosci 2015;3:234–7.Article
- 15. Yi HA, Lee SR, Lee H, Ahn BH, Park BR, Whitman GT. Sudden deafness as a sign of stroke with normal diffusion-weighted brain MRI. Acta Otolaryngol 2005;125:1119–21.ArticlePubMed
Citations
Citations to this article as recorded by





 KBS
KBS
 PubReader
PubReader ePub Link
ePub Link Cite
Cite